Does Medicare Require Prior Authorization For Surgery
This does not change any medical necessity or documentation requirements. The MA 97 Prior Authorization Request Form can be printed from the Medical Assistance Forms web page or ordered off of the MA 300X - Medical Assistance Provider Order Form PDF download.
Https Www Michigan Gov Documents Mdhhs Professional Billing Tip Prior Authorization 09 25 2017 602029 7 Pdf
Prior Approval PA Criteria For Surgical Procedures Many procedure codes require prior authorization PA before reimbursement will be made by the Medicaid program.
Does medicare require prior authorization for surgery. This new ruling does not impact ambulatory surgical center ASCs. This new requirement will necessitate physicians and hospitals to work together to get PA approval to avoid patient access disruptions. If you are a network provider who is contracted directly with a delegated medical groupIPA then you must follow the delegates protocols.
Botulinum toxin injections or Botox Injections used to treat muscle disorders like spasms and twitches. PAs can be submitted to the Medicare Administrative Contractor MAC as early as June 17 so procedures planned in July will have already received. The list mostly includes durable hospital equipment and prosthetics.
Effective July 1 2020 prior authorization PA is required for hospital outpatient departments HOPD when any of the following eyelid surgeries or Botox injections performed. However it is your responsibility to make sure that you have prior authorization before receiving certain health care procedures services and prescriptions. This is extremely important to know especially for people being treated for cancer.
Medicare including Part A rarely requires prior authorization. Call your insurance company before you receive your health care services or prescription. Medicare does not cover cosmetic surgery or expenses incurred in connection with such surgery.
Medicare requires prior authorization before you get these hospital outpatient services that are sometimes considered cosmetic. Prior authorization helps to ensure that all applicable Medicare coverage payment and coding rules are met before a service is furnished. The provider or beneficiary must include the UTN on the claim submitted to Medicare for payment.
Blepharoplasty Surgery on your eyelid to remove droopy fatty or excess tissue. Discuss the health care services or prescription that you need and ask if prior authorization is required. If the provider is seeking payment from Medicare as a secondary payer for an applicable hospital OPD service prior authorization is required.
If it does you can obtain the forms to send to Medicare from your hospital or doctor. By making prior authorization compulsory the agency hopes to avert incorrect payments when the purpose of the surgery is cosmetic and assure that patients are covered when the purpose is functional. Health insurance companies use the prior authorization or pre-approval process to verify that a certain drug procedure or service is medically necessary BEFORE it is done or the prescription is filled.
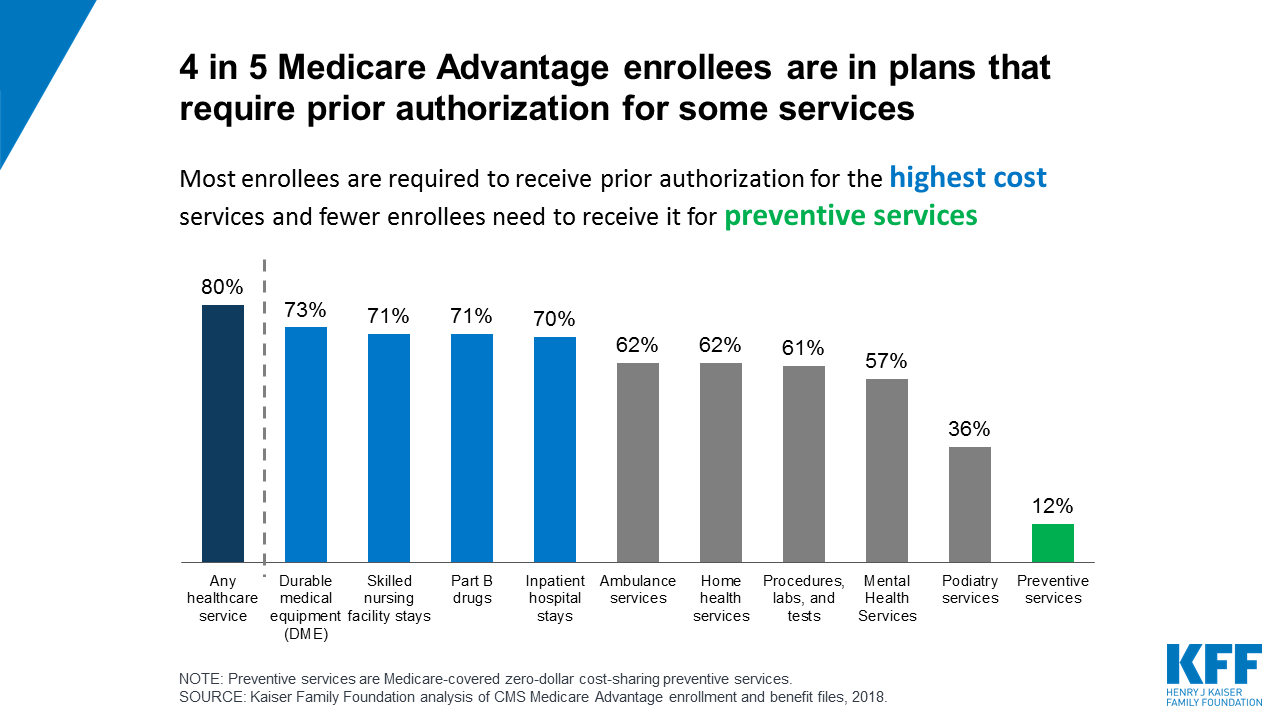
Providers who plan to perform both the trial and permanent implantation procedures using CPT code 63650 in the OPD will only require prior authorization for the trial procedure. Medicare Advantage policyholder may have encountered a pre-authorization requirement a process that is used in the large majority of Medicare Advantage plans according to the Kaiser Family. If a prescription requires authorization the pharmacy will contact whoever prescribed the medication physician and will let the physicians know the insurance company requires a PA.
They must meet the same regulatory and accreditation requirements as UnitedHealthcare. Next the physician will contact the insurance company they will have to fill out forms and submit a formal. Visit the Preauthorization and notifications list online.
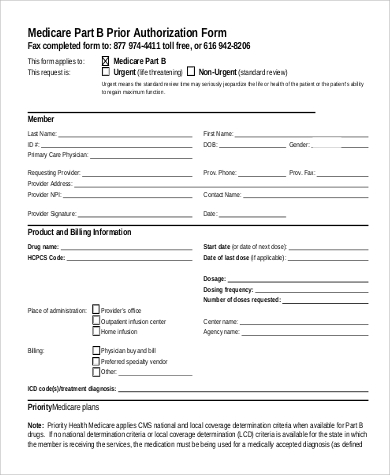
Medicare Part B Prior Authorization. Health care providers usually initiate the prior authorization request from your insurance company for you. Under prior authorization the provider submits a prior authorization request PAR and receives a decision prior to rendering services.
Effective July 1 2021 Medicare will require prior authorization PA for Spinal Cord Stimulation SCS percutaneous leads implanted during procedures performed in outpatient hospitals. First Coast will begin accepting prior authorization requests PARs for the following hospital outpatient department OPD services on June 17 2020 for services provided beginning on or after July 1 2020. The Centers for Medicare Medicaid Services CMS has seen an increase in HOPD surgeries that depending on the circumstances can qualify as either functional or cosmetic.
For certain medical procedures services or medications your doctor or hospital needs advanced approval before your plan covers any of the costs. When the trial is rendered in a setting other than the OPD providers will need to request prior authorization for CPT code 63650 as part of the permanent implantation procedure in the hospital OPD. Each MA plan has different requirements so MA enrollees should contact their plan to ask whenif prior authorization is needed.
Medical authorizations Does this service require preauthorization. The PAR must include all. Retroactive authorization is not normally granted on a routine basis.
Prior authorization is not required for emergency or urgent care. The MA 97 - Outpatient Services Authorization Request form is used to request a medical servicesupply that requires prior authorizationprogram exception. However it is possible to obtain such approval on a case-by-case basis.
Delegates may use their own systems and forms. Medicare Advantage MA plans also often require prior authorization to see specialists get out-of-network care get non-emergency hospital care and more. At this stage the patient can choose to pay the prescription themselves or wait for authorization from the insurers.

Medicare To Require Prior Authorization For Certain Outpatient Department Services Starting July 1 2020
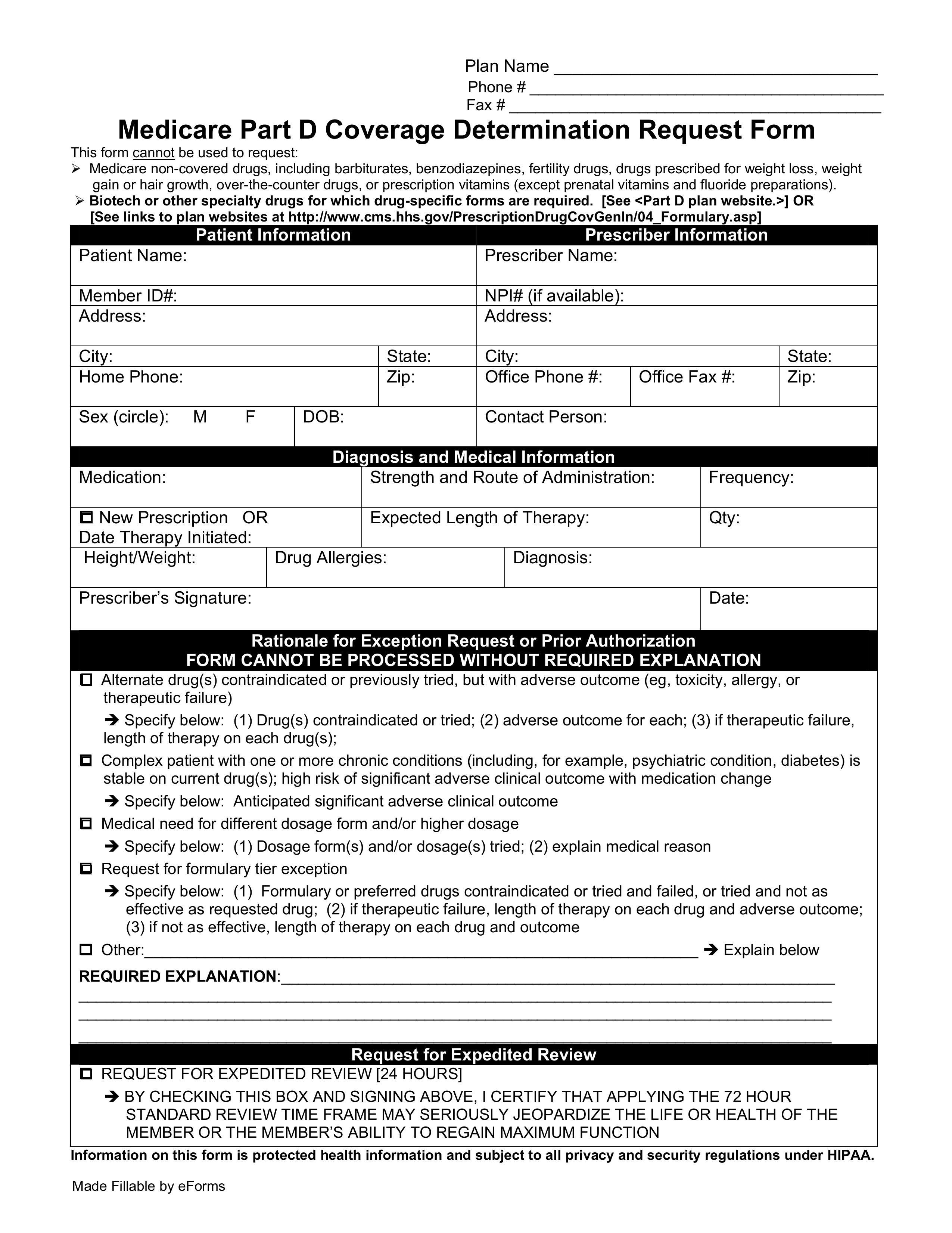
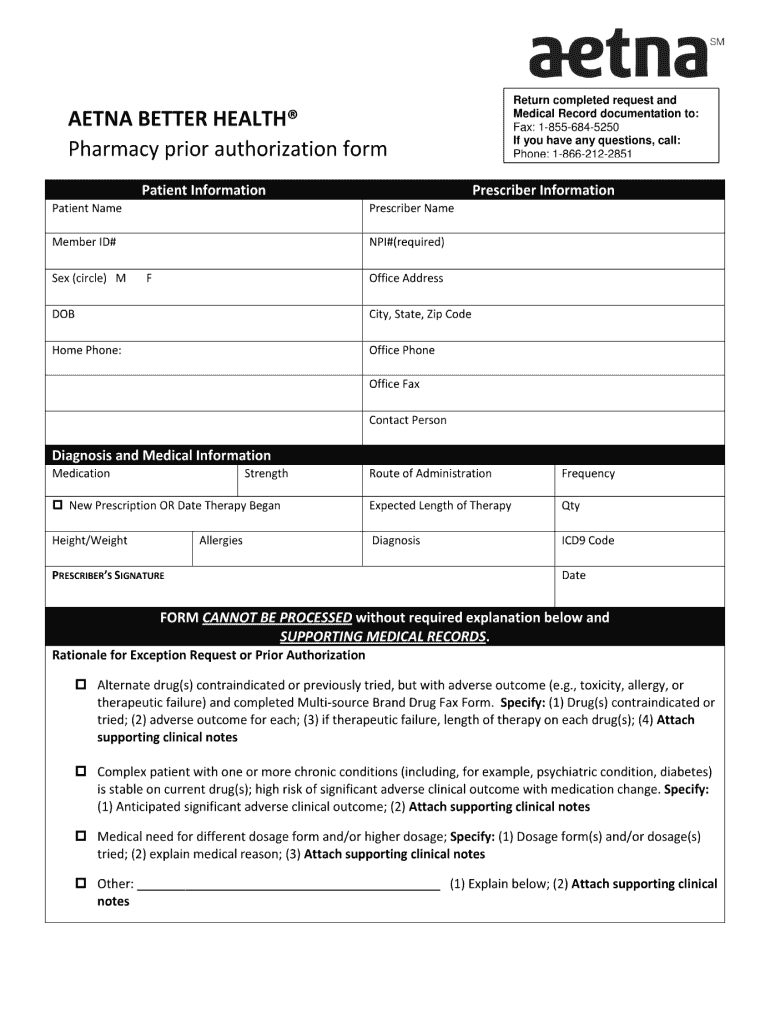
Free Medicare Prior Rx Authorization Form Pdf Eforms
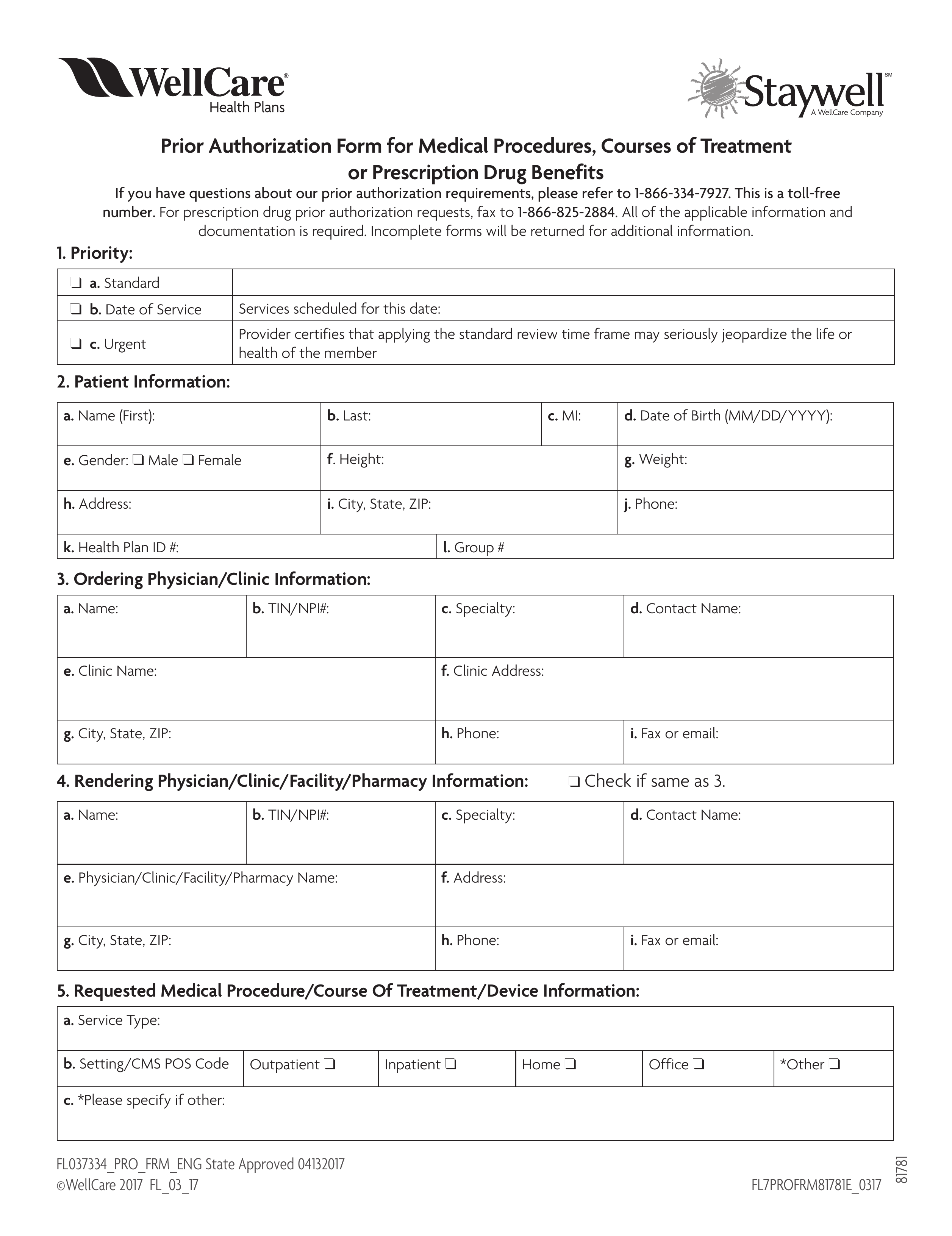
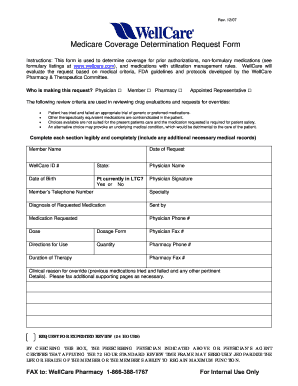
Free Wellcare Prior Rx Authorization Form Pdf Eforms
Https Www Magellanhealth Com Media 17894 Acny Priorauthreqsrvcs Pdf
Https Www Fideliscare Org Portals 0 Providers Authorizationgrids Medicare Authorization Grid Effective January 2021 Pdf
Https Www Uhcprovider Com Content Dam Provider Docs Public Prior Auth Cardiology Faq Cardiology Prior Auth Program For Uhc Medicare Advantage Pdf
Http Www Molinahealthcare Com Providers Mi Medicaid Forms Pdf Mi Prior Authorization Guide 8 1 Pdf
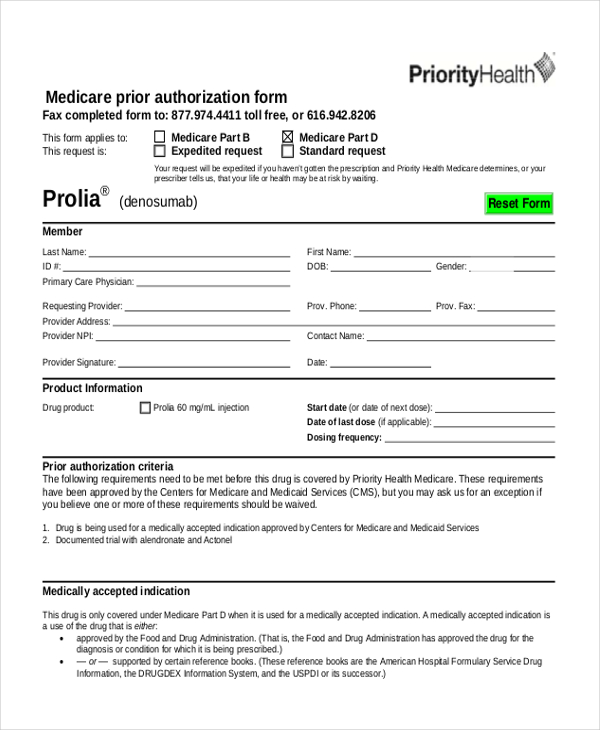
Free 8 Sample Prior Authorization Forms In Pdf Ms Word

Medicare Prior Authorization Explained Medicarefaq
Meridian Rx Prior Auth Form Fill Online Printable Fillable Blank Pdffiller
Https Www Uhcprovider Com Content Dam Provider Docs Public Prior Auth Radiology Faq Medicare Advantage Radiology Prior Authorization Pdf
Free 9 Sample Prior Authorization Forms In Ms Word Pdf
Https Www Floridablue Com Docview Medicare Advantage Musculoskeletal Management Quick Guide For Ordering Physicians December 2015
Https Www Fideliscare Org Portals 0 Providers Authorizationgrids 2020 04 Fideliscare Medicare Authorizationgrid English Pdf
Wellcare Medicare Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Https Www Uhcprovider Com Content Dam Provider Docs Public Prior Auth Pa Requirements Medicare Uhc Medicare Advantage Uhccp Prior Authorization Effective Jan 1 2020 Pdf
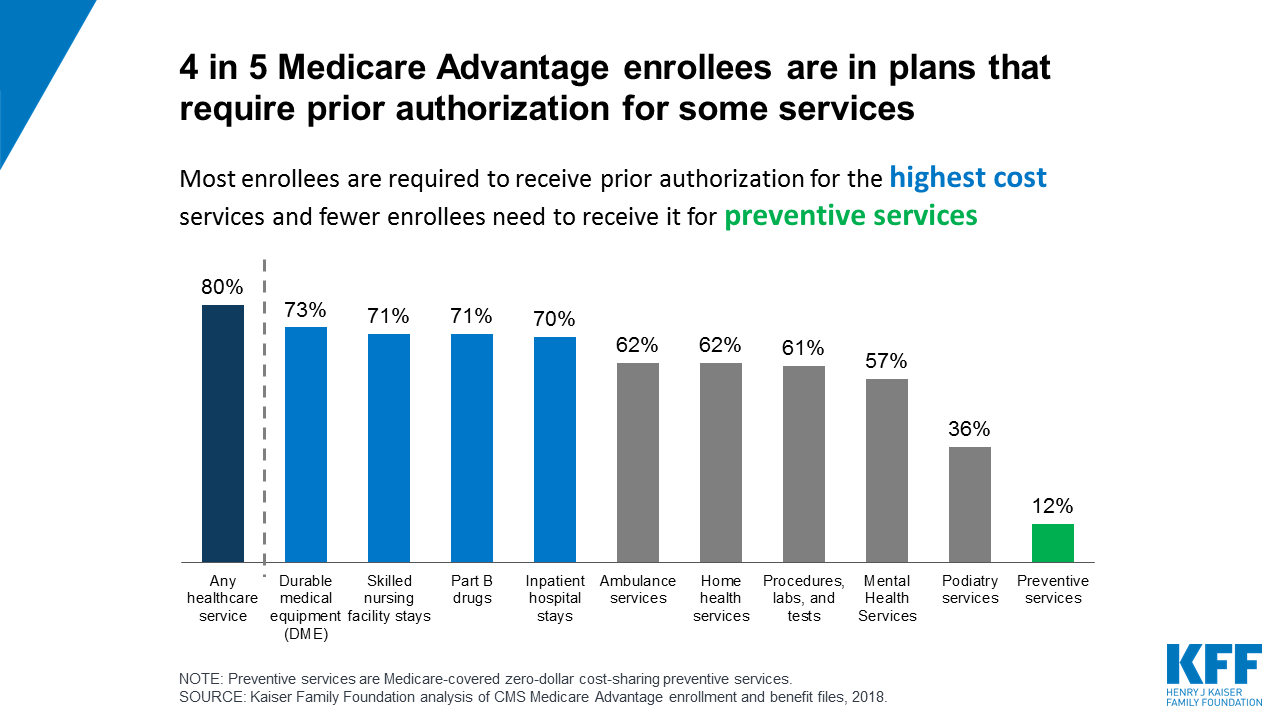
Prior Authorization In Medicare Advantage Plans How Often Is It Used Kff
Https Www Homestatehealth Com Content Dam Centene Home State Health Pdfs 2020 20medicare 20prior 20authorization 20code 20listing 20revised Pdf
Https Www Uhcprovider Com Content Dam Provider Docs Public Prior Auth Pa Requirements Medicare Uhc Medicare Advantage Uhccp Prior Authorization Effective 1 1 2021 Pdf
Post a Comment for "Does Medicare Require Prior Authorization For Surgery"